
Judy Van De Veen, 36, plays with her daughter, Cheyenne, in Gillette, N.J. Van De Veen has struggled for years with an eating disorder and alcohol abuse.
Another eating disorder is now making headlines: Drunkorexia.
Doctors are now seeing a disturbing new eating disorder among college-age women: self-imposed starvation combined with alcohol abuse.
From The New York Times
March 2, 2008
Starving Themselves, Cocktail in Hand
By SARAH KERSHAW
MANOREXIA. Orthorexia. Diabulimia. Binge Eating Disorder
All are dangerous variations on the eating disorders anorexia and bulimia, and have become buzzwords that are popping up on Web sites and blogs, on television and in newspaper articles. As celebrity magazines chronicle the glamorous and the suffering, therapists and a growing number of researchers are trying to treat and understand the conditions.
The latest entry in the lexicon of food-related ills is drunkorexia, shorthand for a disturbing blend of behaviors: self-imposed starvation or bingeing and purging, combined with alcohol abuse.
Drunkorexia is not an official medical term. But it hints at a troubling phenomenon in addiction and eating disorders. Among those who are described as drunkorexics are college-age binge drinkers, typically women, who starve all day to offset the calories in the alcohol they consume. The term is also associated with serious eating disorders, particularly bulimia, which often involve behavior like bingeing on food — and alcohol — and then purging.
Anorexics, because they severely restrict their calorie intake, tend to avoid alcohol. But some drink to calm down before eating or to ease the anxiety of having indulged in a meal. Others consume alcohol as their only sustenance. Still others use drugs like cocaine and methamphetamine to suppress their appetites.
“There are women who are afraid to put a grape in their mouth but have no problem drinking a beer,” said Douglas Bunnell, the director of outpatient clinical services for the Renfrew Center, based in Philadelphia.
The center, like a small but growing number of eating-disorder and addiction-treatment facilities, most on the West Coast, offers a dual focus on substance abuse and eating disorders.
Dr. Bunnell, the past president of the National Eating Disorders Association, said the obsession with being skinny and the social acceptance of drinking and using drugs — along with the sense, lately, that among celebrities, checking into rehab is almost a given, if not downright chic — are partly to blame.
“Both disorders are behaviors that are glorified and reinforced,” Dr. Bunnell said. “Binge drinking is almost cool and hip, and losing weight and being thin is a cultural imperative for young women in America. Mixing both is not surprising, and it has reached a tipping point in terms of public awareness.”
Psychologists say that eating disorders, like other addictions, are often rooted in the need to numb emotional pain with substances or the rush provided by bingeing and purging. The disorders are often driven by childhood trauma like sexual abuse, neglect and other sources of mental anguish.
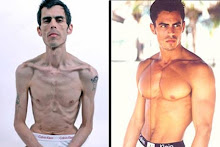
Manorexia is the male version of anorexia. Orthorexia is an obsession with what is perceived as healthy food — eliminating fats and preservatives, for example. But people with this condition can dangerously deprive themselves of needed nutrients.
Diabulimia refers to diabetics who avoid taking insulin, which can cause weight gain, in order to control their weight. Despite the name, the disorder does not typically involve purging.
Binge Eating Disorder refers to obsessive overeating, especially of foods high in salt and sugar, that does not involve excessive exercise or purging to compensate for the high caloric intake.
Judy Van De Veen, 36, who lives in Gillette, N.J., became anorexic at 24. She said she starved herself, meting out small bites of low-calorie food for two months. Then she began bingeing and purging, throwing up entire boxes of cereal, whole pizzas and fast food from drive-throughs that sometimes cost her $80 a day.
She went into treatment, both inpatient and outpatient, for her eating disorder for several years in the late 1990s, with mixed results. In 2001, still struggling with bulimia, she took up drinking. If she ate while drinking, she said, she would purge, but then consume more alcohol to make up for the loss, because she wanted to remain drunk.
Many bulimics who drink use alcohol to vomit, experts on eating disorders say, because liquid is easier to purge. They also tend to vomit because they often drink on empty stomachs.
“In the beginning of my eating disorder I wouldn’t touch alcohol because it is so high in calories,” said Ms. Van De Veen, who later found herself regularly hospitalized for dehydration. “But I have the disease of more: I just want more no matter what it is.”
Two years into her drinking problem, she joined a 12-step program. She spent the next two years in and out of six residential rehab programs, spending about $25,000 of her own money because she didn’t have health insurance. But none of the programs were equipped to address eating disorders, so she binged and purged and her eating disorder raged.
Ms. Van De Veen said she has been sober for three years, but is still struggling with bulimia. She now has a 14-month-old daughter, Cheyenne, and she said that her pregnancy and support groups had helped her make progress on her eating disorder.
“I had an excuse to eat,” she said of being pregnant. “I didn’t care and I loved it.”
But she said the temptation to binge and purge is haunting her again.
Trish in Philadelphia has struggled for years with an eating disorder and alcohol abuse. She recently checked into a treatment centre.
Trish, 27, who has had an eating disorder for the last 10 years, recently checked into Renfrew, her fifth stint in a treatment center or hospital.
Like Ms. Van De Veen, Trish, who agreed to be interviewed on the condition that only her first name be used to protect her privacy, struggled with anorexia first and then found alcohol. Before she was admitted to Renfrew, she said she was blacking out from lack of food and suffering from excruciating stomach pain.
Trish, a nurse who lives in Ohio and works with cardiac patients, said she would starve herself through her 8- or 12-hour shifts, staring at the clock and fixating on when she could have her first drink. Drinking, she said, relaxed her when she had to eat in front of other people, a huge source of stress.
“The alcohol is probably what kept any weight on me,” she said in an interview late last month at the Renfrew Center, which she entered on New Year’s Eve for eight weeks of treatment.
“Drinking helped me be less anxious,” she said. “It helped me be more of Trish. The two go together: If I drink more, I’m more into my eating disorder and vice versa.”
Studies show that binge drinking and alcohol abuse are on the rise among women, who are also more prone than men to eating disorders.
About 25 to 33 percent of bulimics also struggle with alcohol or drugs, according to a study published last year in the journal Biological Psychiatry. Between 20 and 25 percent of anorexics have substance abuse problems, the study found.
A growing number of researchers are examining the psychological and neurological links between eating disorders and substance abuse: Does eating a chocolate bar, or bingeing and purging, stimulate the same pleasure centers in the brain as drugs or alcohol?
Suzette M. Evans, a professor of clinical neuroscience at Columbia, recently began a study of the connection between bulimia and substance abuse, a field she said has been neglected.
“People are finally beginning to realize that food can function in the same way as drugs and alcohol,” Dr. Evans said.
As more patients seek treatment for both eating disorders and substance abuse, a complicated set of mixed messages can arise. The response to addiction is abstinence; but quitting food is not an option.
“We’re trying to get our patients to find effective behaviors and life skills,” said Dr. Kevin Wandler, the vice president for medical services at Remuda Ranch, which addresses both eating disorders and addiction at its facilities in Arizona and Virginia.
“Eating normally would be an effective behavior, but it’s easier to give up alcohol and drugs because you never need it again,” Dr. Wandler said. “If your drug is food, that’s a challenge.”
Trish left Renfrew on Feb. 22, after her second time in treatment there. She was determined, she said, to break her obsessions with weight, food and alcohol. Before she checked in, “I didn’t even have the energy to laugh,” she said. But as she prepared to go home, she had more hope than she has had in years.
“I will not live my life like this,” she said. “I’ve learned this time not to be ashamed. I want to love myself and I want to forgive myself.” (bolding mine)
LINK:
Follow on Buzz




























2 comments:
Excellent post, Medusa. Very informative. I was just reading about Bulimarexia. I didn't know about these others.
My blog: Weighing The Facts
This is what I have. I thought I was alone! Thanks for posting this!
Post a Comment